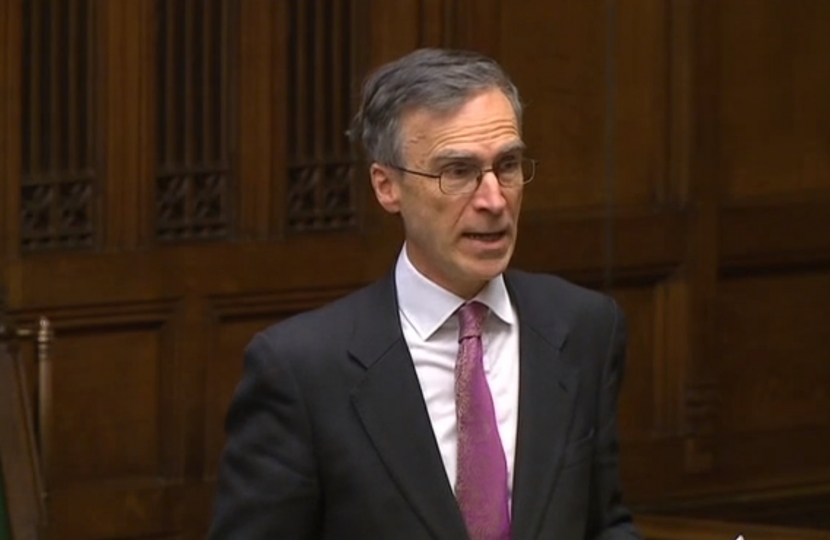
This afternoon, Andrew delivered a speech in the House of Commons on the issue of the NHS winter crisis.
Andrew said:
'It is a great pleasure to follow the hon. Member for Stockton South (Dr Williams), who qualified in 1996. I have about 10 years on him, and since 1984 I cannot recall a winter when there was not talk of pressure. We have to understand that this is not a new phenomenon. I particularly recall the bad winter of 2009, and the very positive way in which the then Opposition approached it and helped the then Government, in the interests of not politicising and not weaponising this issue. It is pity we have not seen the same thing repeated.
'We need to give due credit to managers in the NHS. They come in for a lot of flak all the time, but we have seen a managed process this year and it has taken a great deal of input to make sure we do the best we can to disadvantage patients the least; I pay tribute to that much-maligned group. The only way in which I can see we can make this better is by running a lower bed occupancy rate, which is okay but it has opportunity costs attendant upon it. The reality of doing such a thing, which would avoid the sort of cancellations we have seen this winter, as in any winter, is severe, and I do not think many right hon. or hon. Members would wish to see those things.
'That brings me on to the Commonwealth Fund, which was rightly cited by the Prime Minister earlier in response to my question in Prime Minister’s questions. She was right to say that on access, equity, the care process and administrative efficiency—four of the five points the Commonwealth Fund looks at—the NHS does very well. The problem is with the last one, which is clinical outcomes, where we run 10th out of 11, with the 11th being the United States of America, which nobody here wishes to emulate. We do not do well on clinical outcomes—we do not do well on cancer, on stroke or on heart attack—and we need to do something about it. It is no good citing OECD averages. We need to be comparing ourselves with Denmark, Germany, France and the Netherlands, not with the basket of countries included in the OECD.
'Where does all that lead us? It leads us to a debate about resources. Having talked about management, which is vital, we need to address long-term resources. I entirely support those who wish planning to be done on a 10-year rather than five-year basis. That is vital, and we must also ensure that we have the necessary funding for the improvements we need to achieve to get outcomes up to the level enjoyed by our peer-group nations in western Europe, not the basket of nations with which we are often erroneously compared. How do we do that? We have to take the public with us and work across party boundaries. None of the decisions that will ultimately be made about the future of our national health service in this, its 70th anniversary year, are necessarily going to be easy. It is important that we at least try to get some level of cross-party consensus. We can do that by establishing a body that is above politics. The route to which I am drawn is the establishment of a royal commission, with all its problems.
'The Merrison commission 40 years ago was the last big royal commission that considered matters to do with the health service. It came in for a lot of criticism, but most of its recommendations, made 40 years ago, were ultimately rolled out into Government policy. With the right terms of reference, such a body would be effective. That seems to me to be the right and proper way to deal with the future, particularly the sustainable funding future of our most treasured of national institutions. I very much hope that my Front-Bench colleagues will listen to those of us from all parties—particularly the recommendation from the Centre for Policy Studies this week—who think we should set up a royal commission in this 70th anniversary year to consider the future of our national health service.'
